Just because a bill has been paid, doesn't mean it's the end of the story.
80%
The Number of medical bills that contain some kind of error

High-powered Analytics
Audxguard
WellRithms provides insights for your health plan's financial performance via its post-payment product, Audxgaurd
Audxguard
Audxguard Claim Review
- Leverages claims data to reveal plan performance insights and reduce fiduciary liability

Shield Indemnification™
Guaranteeing our recommended payment amount
Shield Indemnification™ protects carriers, plans, and members from the adverse impact of litigation expenses and balance billing tactics.
We are backed by a captive insurance company that allows for the transfer of all legal and financial liability from the payor to WellRithms, thereby guaranteeing the recommended payment amount.
Featured Insights
Exposing Trauma Response Charges
Bill of the Month
A California-based hospital recently submitted a bill of $100,618 for a one-night stay, all centered around a treatment for a fractured…
Medical Overbilling: Examining the Heart of the Problem
Bill of the Month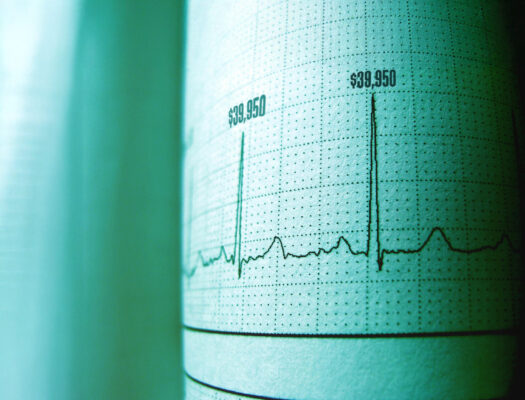
A two-day hospital stay in a California-based hospital gave our bill review team some serious heart palpitations – not from medical…
WellRithms Recognized as a Rising Star in BenefitsPRO’s 2024 Luminaries Awards
BlogWe are honored that WellRithms has been named to BenefitsPRO Luminaries Class of 2024 in the Rising Star category. This recognition…
Want to work with WellRithms?
Let’s connect to find a solution best for you and your team.